1. What Are SOAP Notes in Massage Therapy?
SOAP notes in massage therapy are a structured method of documenting every client session—from the client’s first visit to their latest progress check. This standardized format is widely used across the massage therapy, chiropractic, and wellness industries to ensure consistent, accurate, and professional record-keeping.
If you’ve ever wondered how to write SOAP notes for massage therapists, the process follows a clear, four-part format known as SOAP:
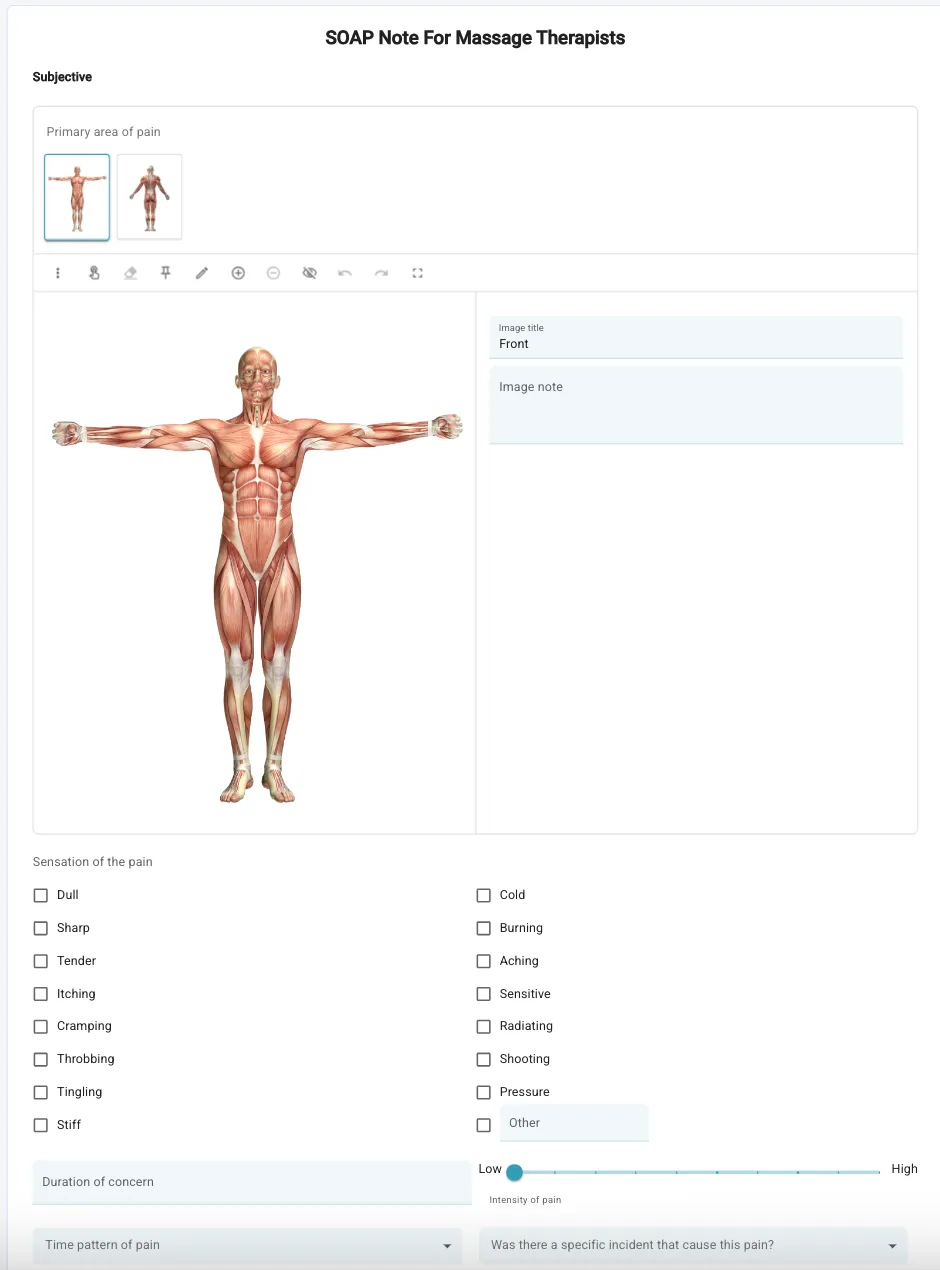
- S – Subjective: What the client reports, including pain level, areas of tension, or specific wellness goals.
- O – Objective: What the massage therapist observes—such as muscle tightness, posture, skin temperature, or range of motion limitations.
- A – Assessment: The therapist’s analysis of the findings, identifying underlying issues like postural strain, fascial restrictions, or trigger points.
- P – Plan: The treatment plan, recommended techniques (e.g., deep tissue, Swedish, or myofascial release), and follow-up care instructions or home exercises.
This SOAP note documentation for massage therapists provides a consistent framework to track each client’s progress over time and support massage therapy progress notes that meet both professional and insurance standards.
Whether you’re running a solo practice or part of a multidisciplinary wellness clinic, detailed SOAP notes help ensure continuity of care, professional accountability, and compliance with massage therapy documentation requirements. They also make collaboration with chiropractors, physiotherapists, and healthcare providers seamless—especially when using digital SOAP note software designed for wellness clinics and medical massage billing.
💡 Tip: Using a SOAP note template or digital SOAP note system helps you streamline your massage documentation process, save time after each session, and maintain HIPAA-compliant client records.
2. When Should Massage Therapists Use SOAP Notes?
Massage therapists should create SOAP notes immediately after every session to ensure accurate documentation, continuity of care, and consistent client progress tracking. Writing your SOAP notes right away helps you remember the client’s exact feedback, muscle response, and any adjustments made during treatment—critical details that can easily be lost if delayed.
SOAP notes play a key role in massage therapy record keeping and should be part of your daily workflow, whether you specialize in relaxation massage, therapeutic massage, or medical massage treatments.
Common Situations When SOAP Notes Are Essential
Initial Consultation
During a client’s first visit, SOAP notes help establish a clear foundation for future care. Document the client’s reported symptoms, pain scale, health history, and treatment goals. This creates the baseline that every future massage therapy progress note will refer back to.
Session Follow-Ups
After each session, update your SOAP notes to record how the client responded to treatment. Note any changes in muscle tension, range of motion, or pain level. These ongoing updates create a measurable picture of improvement over time and allow you to fine-tune your treatment plan for better results.
Professional Referrals
When working alongside other professionals—such as chiropractors, physiotherapists, or acupuncturists—SOAP notes make it easy to share clear, standardized information. A well-documented SOAP note shows what you observed, the techniques applied, and your clinical reasoning, helping ensure all providers are aligned on the client’s progress and plan of care.
Insurance Documentation
For medical massage or insurance billing, SOAP notes are a must. Insurance companies often require detailed session notes to verify the type of treatment provided, its purpose, and the results achieved. Keeping consistent, professional SOAP note documentation for massage therapy sessions protects your practice and simplifies reimbursement.
Mobile and On-the-Go Practices
If you offer mobile massage therapy, digital SOAP notes are especially valuable. A mobile-friendly SOAP note app lets you document sessions right after each visit—quickly, securely, and without the risk of losing paper records. This is ideal for therapists managing multiple clients or working across several locations.
Why Timely SOAP Notes Matter
Completing SOAP notes promptly after each session helps ensure accuracy, compliance, and professional accountability. Late or incomplete documentation can lead to errors, gaps in care, and even legal complications if a record is requested later.
By keeping up-to-date SOAP notes for every massage therapy session, you not only meet professional standards but also elevate your client experience—showing care, precision, and commitment to lasting results.
3. Why SOAP Notes Matter for Massage Therapists & Wellness Clinics
Documenting SOAP notes in massage therapy isn’t just about compliance—it’s about providing exceptional, evidence-based care that builds client trust and long-term results. Proper SOAP note documentation ensures that every massage session is purposeful, measurable, and aligned with your client’s ongoing goals.
In today’s wellness industry, where professionalism and credibility are essential, consistent SOAP notes set you apart as a therapist who values precision, organization, and quality care. They reflect your commitment to both client wellbeing and business professionalism.
Enhance Client Results
Detailed SOAP notes help you track client progress over time—from the first appointment to the most recent session. You can identify which techniques provide the best relief, how pain levels change, and what adjustments are needed to keep improving outcomes. This process allows massage therapists to deliver more personalized, goal-oriented treatments that create measurable improvement and client satisfaction.
Support Insurance Billing and Medical Documentation
For therapists who provide medical or rehabilitative massage, SOAP notes are essential for insurance documentation. Clear, structured records demonstrate medical necessity and verify treatment details for reimbursement. Organized SOAP note documentation also helps protect your practice during audits and shows that you meet healthcare-level standards of professionalism.
Improve Client Retention and Experience
Keeping detailed massage therapy progress notes lets you remember client preferences, pain triggers, and pressure sensitivities from past visits. This attention to detail helps clients feel cared for and understood. When a therapist can recall exactly what worked before, it builds trust and leads to stronger long-term relationships, better rebooking rates, and consistent retention.
Demonstrate Professionalism and Build Trust
Well-structured SOAP notes show clients—and other health professionals—that your work follows a professional and accountable standard. They make collaboration easy in multidisciplinary clinics, allowing chiropractors, physiotherapists, and acupuncturists to understand your findings and continue treatment seamlessly. Thorough documentation elevates your reputation and sets your practice apart as credible and well-organized.
Legal and Ethical Protection
Accurate SOAP notes protect both you and your clients. In case of a dispute or complaint, your documentation serves as a legal record of what was discussed, observed, and performed in each session. Maintaining clear massage therapy records also ensures ethical transparency and compliance with local regulations, safeguarding your business from potential liability.
When SOAP notes are consistent, structured, and securely stored, they do more than meet standards—they improve the quality of care, enhance team communication in wellness clinics, and strengthen the overall professionalism of your practice. SOAP notes turn ordinary session records into a vital tool for growth, accountability, and client success.
4. SOAP Format Explained: Subjective, Objective, Assessment, Plan
Each part of a SOAP note serves a distinct purpose. Here's how to write each one effectively:
Subjective (S)
- “Where do you feel discomfort today?”
- Client’s own description of pain/tension
- Duration, onset, and severity of symptoms
- Pain scale rating (0–10)
Objective (O)
- Postural imbalances observed
- Palpation results (tightness, texture, temperature)
- ROM tests (if applicable)
- Muscle tone and symmetry
Assessment (A)
- Interpretation of findings from S + O
- Response to previous treatment
- Hypotheses about client condition (e.g., trigger point involvement, fascial restrictions)
Plan (P)
- Techniques applied (e.g., trigger point, deep tissue)
- Areas of focus and rationale
- Recommendations: stretches, hydration, next visit timing
Tip: Use consistent terminology and be as specific as possible.
5. Massage SOAP Note Example (Real-World Case)
Here’s a simple massage SOAP note example:
S: Client reports tension in upper shoulders and neck. Describes it as a "dull ache" worsening after desk work. Rates it 6/10.
O: Forward head posture, limited cervical rotation. Palpation reveals tight upper trapezius and levator scapulae bilaterally.
A: Postural strain due to prolonged sitting.
P: 30 minutes of trigger point release and myofascial work. Client advised to perform neck stretches daily. Rebook in 1 week.
This clear example shows how each component flows into the next to support a personalized treatment plan.
6. SOAP Notes for Massage Example Template (Downloadable)
Use this easy template to streamline your massage SOAP notes:
S: Client reports...
O: Observed...
A: Assessed as...
P: Plan to...
🎁 Download Your Free Massage SOAP Notes Template
Everything you need to document your sessions professionally—includes a massage documentation template and a real SOAP note example. Get it now
7. Chiropractic SOAP Note Example (With Key Differences)
S: Patient reports mid-back stiffness after gym injury. Rates pain 5/10.
O: Restricted thoracic extension. Positive Kemp's test.
A: Facet joint irritation.
P: Thoracic manipulation + ice therapy. Reassess in 2 days.
Compared to massage notes, chiropractic SOAP notes emphasize clinical testing and alignment patterns.
Let's get to know each other
Keep your clients coming back.
8. SOAP Notes for Chiropractors vs. Massage Therapists
9. Common SOAP Note Mistakes to Avoid
- ❌ Writing vague descriptions (e.g., “client feels tight”)
- ❌ Skipping the Assessment or Plan section
- ❌ Not including at-home recommendations
- ❌ Using inconsistent terminology
- ❌ Failing to update notes from session to session
Consistency and specificity are what make SOAP notes powerful.
10. Digital SOAP Notes vs. Paper Notes
Digital notes are ideal for solo providers and large clinics alike.
11. HIPAA Compliance and Documentation Retention
SOAP notes contain Protected Health Information (PHI), so proper storage is legally required.
Best Practices:
- Encrypt and password-protect digital records
- Store notes for 7–10 years (depending on your jurisdiction)
- Obtain client consent when sharing notes
- Avoid storing paper notes in unsecured locations
12. AI and SOAP Notes: The Future of Documentation
AI is streamlining documentation in the wellness industry.
How AI Helps:
- Voice-to-text entry for hands-free note-taking
- Predictive templates based on prior sessions
- Auto-fill of common treatments per client profile
- Intelligent tagging for symptoms and services
AI doesn’t replace your expertise—it multiplies your efficiency.
13. How to Use SOAP Notes to Improve Client Outcomes
SOAP notes aren’t just for recordkeeping—they’re tools for transformation:
- Track how a client’s pain scale changes over time
- Adjust your treatment plan based on what works
- Empower clients with personalized feedback
- Collaborate easily with chiropractors, physiotherapists, and more
This leads to better outcomes, stronger trust, and repeat business.
14. Choosing the Best SOAP Note Software (and EHR for Massage Therapists)
Finding the right SOAP note software is one of the most important decisions for any massage therapist, spa owner, or med-spa clinic director. The ideal platform does far more than store notes — it becomes your complete practice management hub, connecting your documentation, appointment scheduling, client communication, and billing into one seamless workflow.
Whether you operate a solo massage practice, manage a busy day spa, or run a multi-location medical spa, the best SOAP note software should help you stay organized, compliant, and efficient while saving time between sessions.
Mobile-Friendly SOAP Note Charting
In 2025, flexibility is everything. Choose a cloud-based SOAP note system that allows you to chart on any device — desktop, tablet, or phone. A mobile SOAP note app makes it easy to document sessions immediately after treatment, ensuring accuracy and compliance while you’re on the go.
For massage therapists offering mobile or in-home services, a mobile-friendly charting tool prevents lost records and keeps every client file securely backed up in the cloud.
Integrated Intake, Consent Forms & Client Profiles
Look for a digital SOAP note system that automatically links to your client intake and consent forms. This integration lets you pull health history, allergies, treatment goals, and past notes into one secure record — no more cross-checking paper files.
When SOAP notes, digital forms, and treatment plans live in the same ecosystem, your documentation becomes faster, more accurate, and fully HIPAA- and PIPEDA-compliant.
💡 Tip: Platforms like Yocale unify SOAP notes, intake forms, and progress notes, so you can focus on care instead of paperwork.
Appointment Scheduling, Billing & Payments in One Place
The best massage therapy documentation software connects SOAP notes directly with your scheduling and billing tools. This ensures a smooth workflow — from booking to treatment to checkout.
When your SOAP notes, invoices, and receipts are managed in the same EHR system, you eliminate double entry and reduce administrative errors.
For spas and med-spas, this also means staff can track session history, membership usage, and retail sales — all linked to the same client file.
Custom SOAP Templates for Every Practice Type
No two wellness professionals work alike. That’s why customizable SOAP templates are essential.
Choose a system that lets you adjust fields for:
- Massage pressure preferences
- Facial or body treatment zones
- Pain-scale ratings
- Treatment goals or contraindications
- Before-and-after photos
These options make your documentation more relevant and professional for massage therapists, estheticians, and medical spa technicians alike.
HIPAA, PIPEDA & PHIPA Compliance
For med-spa and clinic environments, client data privacy is non-negotiable.
Select SOAP note software that meets HIPAA (U.S.) and PIPEDA/PHIPA (Canada) standards. This ensures all Protected Health Information (PHI) is encrypted, securely stored, and accessible only to authorized users.
HIPAA-compliant SOAP note systems also provide audit trails, user permissions, and secure data backups — protecting both your clients and your business.
Practice Management Software vs. Standalone SOAP Tools
While standalone SOAP apps focus solely on charting, an all-in-one practice management platform combines everything:
- SOAP notes & progress tracking
- Scheduling & online booking
- Digital forms & client records
- Integrated payments & invoicing
- Marketing, retention, and reviews
- Analytics & business reporting
For growing massage and spa businesses, a connected ecosystem is key. You can track progress, automate reminders, and access real-time performance insights — all without switching between tools.
Why Choose an All-in-One System Like Yocale
Yocale’s all-in-one practice management software brings SOAP notes, scheduling, payments, and marketing together under one roof. It’s designed specifically for massage therapists, spas, wellness centers, and med-spas that want to simplify operations and grow with confidence.
With Yocale, you can:
✅ Create and store SOAP notes securely from any device
✅ Attach digital intake forms and before/after photos
✅ Automate appointment confirmations and receipts
✅ Generate reports on treatments, rebookings, and revenue trends
✅ Maintain full HIPAA and PIPEDA compliance
For modern wellness professionals, Yocale makes documentation simple, secure, and scalable — so you can focus less on admin and more on helping your clients feel their best.
Want more inspiration?
Explore:
- Chiropractic SOAP Notes
- Acupuncture SOAP Notes
- General SOAP Note Best Practices
- Uncommon SOAP Note Strategies for Medspas and Wellness Clinics
Simplify SOAP Notes and Client Documentation with Yocale
With Yocale’s built-in SOAP note library, you already have access to everything you need to document your sessions professionally — from customizable massage, spa, and med-spa templates to secure digital intake forms, progress tracking, and HIPAA-compliant client charts.
🎥 Watch how it works: Yocale SOAP Notes Demo
See how easy it is to create SOAP notes, manage appointments, and streamline your entire workflow — all in one platform designed for wellness professionals.
👉 Sign up today for free (no credit card required) or Book a demo with our team to experience Yocale in action.
15. Frequently Asked Questions (FAQ)
1. What are SOAP notes in massage therapy?
SOAP notes are structured documents used by massage therapists to record each client session in a professional, consistent way. They capture four key elements:
- Subjective: The client’s self-reported symptoms or concerns.
- Objective: The therapist’s observations or findings.
- Assessment: The therapist’s analysis and interpretation.
- Plan: The treatment provided and recommended next steps.
Proper SOAP note documentation ensures continuity of care, supports insurance billing, and enhances overall client trust and professionalism.
2. How often should massage therapists write SOAP notes?
Massage therapists should write a SOAP note after every session, regardless of whether it’s a first-time visit or a routine follow-up. Writing notes immediately after treatment ensures all observations, pain levels, and progress updates are captured accurately and completely.
Many therapists now use digital SOAP note software or cloud-based EHR systems to streamline the process and prevent data loss.
3. Are SOAP notes legally required for massage therapy?
Yes, in many regions SOAP notes are legally required—especially for medical or rehabilitative massage and insurance reimbursement claims. Even for relaxation or spa treatments, maintaining clear SOAP notes demonstrates professionalism and protects your business from potential disputes or complaints.
Proper documentation also ensures compliance with HIPAA or PIPEDA regulations, depending on your country.
4. How are SOAP notes different from massage therapy progress notes?
SOAP notes follow a structured, medical-style format, while progress notes may include a broader summary of a client’s overall improvement across multiple sessions.
SOAP notes document one session in detail; progress notes show trends, patterns, and long-term outcomes.
Most practice management systems now allow therapists to create both SOAP and progress notes digitally for comprehensive tracking.
5. What is an example of a SOAP note for massage therapy?
Here’s a simple example:
S: Client reports lower back pain rated 7/10 after long periods of driving.
O: Tightness and tenderness in the lumbar region; limited range of motion.
A: Chronic lumbar strain with possible muscle imbalance.
P: 60-minute deep tissue session focusing on lower back; recommend heat therapy and follow-up in one week.
This example illustrates how SOAP note documentation provides a full picture of the session and treatment plan.
6. Why are SOAP notes important for wellness clinics?
In multi-therapist or multidisciplinary clinics, SOAP notes ensure that all practitioners—massage therapists, chiropractors, physiotherapists, or acupuncturists—are aligned on client progress.
They create consistency, improve communication, and maintain accurate client histories across the entire clinic.
7. Can SOAP notes be written digitally?
Absolutely. Digital SOAP notes are the modern standard for documentation. Using an electronic health record (EHR) system or practice management software allows you to create, update, and securely store notes from any device.
Digital notes also support automation, searchability, and integration with online booking and billing systems.
8. What’s the difference between EHR and SOAP note software?
SOAP note software focuses on documentation and charting, while an EHR (Electronic Health Record) system is a more comprehensive solution that includes SOAP notes, scheduling, forms, billing, and reporting—all in one place.
For massage therapists, an all-in-one practice management system provides the best value and efficiency.
9. What should be included in a SOAP note for massage therapy?
Each SOAP note should include:
- Client name, date, and session duration
- Subjective details (symptoms, pain rating, goals)
- Objective findings (posture, palpation, muscle tone)
- Assessment (interpretation of findings, response to treatment)
- Plan (techniques used, follow-up, home care)
Adding measurable data like range of motion tests or pain scales makes your notes stronger and more professional.
10. Can I use templates for SOAP notes?
Yes, many therapists use massage therapy SOAP note templates to ensure consistency. Templates can be digital or printable and may include dropdowns for common conditions or techniques.
Modern practice management software like Yocale includes customizable SOAP note templates that align with your practice type—sports, prenatal, medical, or relaxation massage.
11. How do SOAP notes help with insurance billing?
SOAP notes serve as official records that demonstrate the medical necessity of a treatment.
Insurance providers often require SOAP documentation to approve claims for therapeutic or rehabilitative massage sessions.
Accurate SOAP notes also prevent denials and simplify reimbursement.
12. Can clients request copies of their SOAP notes?
Yes. Under privacy laws like HIPAA (U.S.) and PIPEDA (Canada), clients have the right to request a copy of their SOAP notes.
Always provide copies securely—through encrypted email or your EHR portal—and maintain records of the request for compliance.
13. How long should SOAP notes be stored?
Massage therapists should retain SOAP notes and related client records for at least 7–10 years, depending on local regulations.
Digital storage through a secure EHR platform is recommended for long-term compliance and ease of access.
14. Can SOAP notes be shared with other professionals?
Yes, with the client’s written consent, SOAP notes can be securely shared with healthcare partners like chiropractors, physiotherapists, or physicians.
Using encrypted EHR systems ensures all shared records remain private and compliant with health data laws.
15. How do SOAP notes improve client outcomes?
By tracking a client’s progress session by session, SOAP notes allow therapists to adjust treatment plans based on what’s working best.
This data-driven approach leads to more effective results, improved retention, and stronger trust between therapist and client.
16. Are SOAP notes different for chiropractors or acupuncturists?
The core format (Subjective, Objective, Assessment, Plan) stays the same, but chiropractors focus on joint and alignment assessments, while massage therapists emphasize muscle tone and tissue response.
Acupuncturists might include meridian or energy-based assessments within the same SOAP framework.
17. Can AI help with SOAP note writing?
Yes. AI SOAP note generators can automatically suggest content, convert speech to text, or pre-fill standard fields based on past sessions.
This technology helps massage therapists save time while maintaining professional and detailed documentation.
However, always review AI-generated notes for accuracy and personalization.
18. How can SOAP notes protect my business legally?
Accurate SOAP documentation provides a legal record of treatment, protecting you if questions or disputes arise.
Well-written notes demonstrate that you followed proper professional standards, obtained consent, and recorded every client interaction responsibly.
19. What’s the difference between SOAP notes and session summaries?
Session summaries may be brief, informal descriptions for internal use, while SOAP notes are structured medical-style documents.
For professionalism and compliance, always use SOAP notes for official client records.
20. What are massage therapy progress notes, and how do they relate to SOAP notes?
Progress notes provide an overview of a client’s journey across multiple sessions—summarizing long-term changes, responses, and treatment outcomes.
They complement SOAP notes, which capture individual session details.
Together, they form a complete client record, ideal for insurance reporting, treatment analysis, and wellness program tracking.
21. What practice management software is best for SOAP notes?
The best systems combine SOAP documentation with appointment scheduling, billing, and intake forms.
Platforms like Yocale’s all-in-one practice management software are designed for massage therapists and wellness clinics, providing digital SOAP notes, progress tracking, and HIPAA/PIPEDA-compliant record storage—everything you need to run your practice efficiently.
22. How can I make writing SOAP notes faster?
Use custom SOAP note templates, AI-assisted writing tools, and pre-set dropdowns for common issues like shoulder tension or lower back pain.
Digital systems also offer auto-save, pre-filled client data, and cloud sync to simplify your workflow and cut documentation time in half.
23. Can SOAP notes be used for both relaxation and clinical massage?
Yes. Even for relaxation sessions, SOAP notes are useful for tracking client preferences, emotional wellbeing, and treatment responses.
For clinical or medical massage, SOAP notes become essential for insurance documentation and communication with other healthcare providers.
24. What’s the best format for SOAP notes in 2025?
The best SOAP note format is digital, cloud-based, and fully customizable.
It should integrate with your practice management software, include secure client storage, and allow access from any device.
In 2025 and beyond, EHR-driven SOAP note systems are the gold standard for efficient, compliant documentation.
Want more examples? See our guides for chiropractic SOAP notes, acupuncture SOAP notes, and medspa SOAP note strategies.




